Patellofemoral Stabilisation Surgery
What is the Patella?
The Patella or Kneecap is a protective bone attached to the quadriceps muscles of the thigh by the quadriceps tendon.
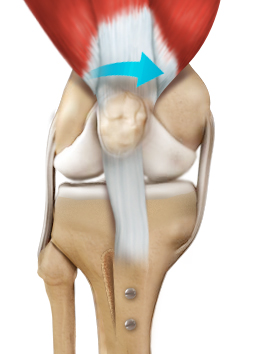
The patella attaches to the femur bone and forms a patellofemoral joint. The patella is protected by a ligament that secures the kneecap from gliding out, called the Medial Patellofemoral Ligament (MPFL).
What is Patellar Dislocation?
Dislocation of the patella occurs when the patella moves out of the patellofemoral groove (called trochlea) onto a bony head of the femur.
If the kneecap partially comes out of the groove, it is called a subluxation; if the kneecap completely comes out, it is called a dislocation.
Patella dislocation is commonly observed in young athletes between 15 and 20 years and affects women because of specific anatomical variations in this group.
What is Patellofemoral Stabilisation Surgery?
Patella stabilisation, also known as Patellar Stabilisation surgery, is a broad term to describe surgery used to stabilise (prevent dislocation) the kneecap (patella).
This procedure aims to restore the normal alignment and movement of the patella, preventing it from dislocating.
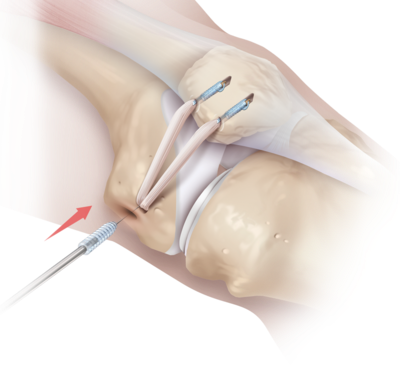
The procedure involves reconstructing the Medial Patellofemoral Ligament, the main stabiliser of the patella and frequently torn when a patella dislocation happens. Usually, sutures, screws, or suspensory fixation devices are employed during the reconstruction. This is called a Soft Tissue Procedure to stabilise the patella.
There are also called adjuvant Bony Procedures involved when bony abnormalities are present, and this important risk factor needs to be corrected.
These surgeries include:
- Tibial Tuberosity Transfer (Triple T)
- Distal Femoral Osteotomies (DFO)
Who is Suitable for Patellofemoral Stabilisation?
Patellofemoral stabilisation is suitable for patients who have experienced recurrent patellar dislocations. It is also an option for patients with patellofemoral instability, which is characterised by a sensation of the kneecap giving way, especially during activities such as running or jumping. Patients with patellofemoral pain syndrome or chondromalacia patellae may also sometimes benefit from Bony Procedures.
What are the Benefits of Patellofemoral Stabilisation?
Patellofemoral stabilisation can offer numerous benefits to patients, including
- Improved Stability: The procedure can improve the stability of the patella, allowing patients to engage in physical activities without the fear of dislocating the kneecap.
- Reduced Pain: Patellofemoral stabilisation can reduce or eliminate pain associated with patellar dislocations or instability.
- Faster Recovery: Patellofemoral stabilisation is a minimally invasive procedure, which means patients can recover faster than with traditional open surgery.
- Long-Term Results: Patellofemoral stabilisation offers long-term results, reducing the risk of recurrent patellar dislocations or instability.
Preoperative Preparation
Preparing for surgery can be overwhelming, both physically and emotionally. However, proper preoperative preparation can help ensure a safe and successful surgery and a smooth recovery.
Medical Clearance
Before surgery, your surgeon will evaluate your medical history and current health status. Depending on your medical history, your surgeon may request medical clearance from your primary care physician or other medical specialists. Medical clearance ensures that you are healthy enough to undergo surgery and reduces the risk of complications.
Preparing for Anesthesia
The type of anaesthesia used for surgery depends on the procedure and the patient's medical condition. Your anesthesiologist will discuss the type of anaesthesia with you and provide instructions on preparing for it. Patients should avoid eating or drinking anything for several hours before surgery to prevent anaesthesia-related complications.
Medications and Supplements
Your surgeon will provide instructions on which medications or supplements to avoid before surgery. Some medications, such as blood thinners, can increase the risk of bleeding during surgery. You must inform your surgeon of any medications or supplements you are taking, including over-the-counter and herbal remedies.
Preparing for After Surgery
Preparing for after surgery is just as crucial as preparing for the surgery itself. Before surgery, arrange for someone to take you home and stay with you for at least 24 hours after surgery. You will also need to arrange for someone to help you with everyday tasks, such as cooking, cleaning, and running errands.
Dietary Preparation
In the days leading up to surgery, it is essential to maintain a healthy and balanced diet to ensure optimal healing after surgery. Eating a diet rich in fruits, vegetables, and lean protein can help promote healing and reduce the risk of complications.
Exercise and Mobility
Physical activity can help reduce stress, improve circulation, and promote healing after surgery. Before surgery, your surgeon will provide safe and beneficial physical activity guidelines. You will be referred to a physical therapist essential in your pre and post-operative rehabilitation. Your outcomes will still depend on how diligent you will be in your rehabilitation.
Mental Preparation
Preparing for surgery can be emotionally challenging. Talking to friends and family, practising relaxation techniques, and seeking support from a mental health professional can help reduce anxiety and stress related to surgery.
Patellofemoral Stabilisation Surgery
The exact details of patellofemoral stabilisation surgery depend on the procedure. The following steps may be involved:
- You will be given general anaesthesia or a nerve block to numb the lower body.
- The surgeon makes a key-hole incision over the knee, typically on the front and a couple of small incisions on the medial side of the knee.
- The surgeon moves the patella aside and may use specialised instruments to arthroscopically release a tight lateral retinaculum, often present.
- Depending on the specific abnormalities present, the surgeon may reconstruct the MPFL, release the lateral retinaculum, and perform a tibial tubercle osteotomy or trochleoplasty.
- Once the reconstruction or realignment is complete, the surgeon closes the incision with sutures, and water-sealed dressings are placed.
After Patellofemoral Stabilisation Surgery
- You will be transferred to the recovery room, where you will be monitored until you are awake and stable.
- You will receive pain medication and anti-inflammatories.
- You will be encouraged to move around as soon as possible, and a physiotherapist will guide exercises to promote healing and mobility.
- A hinge Knee Brace can be recommended, depending on what type of procedures were performed
Post-surgery Care Instructions
After patellofemoral stabilisation surgery, following the post-surgery care instructions provided by your surgeon is essential to ensure proper healing and minimise the risk of complications. Make sure to follow the guidelines.
Rest
Your surgeon will provide specific instructions regarding the duration of rest and the use of crutches or other assistive devices.
Pain Management
Pain and swelling are common after surgery; your surgeon will likely prescribe pain medication to manage these symptoms. Follow the instructions for taking your medication carefully, and contact your surgeon if you have any concerns.
Ice Therapy
Ice is a strong anti-inflammatory that helps manage pain and edema. Especially on the first five days, ice-packed or ice-compressive devices (Game Ready ) are encouraged. Never applied directly to the skin to avoid thermal injuries. Twenty minutes every second hour should be enough.
Physical Therapy
Your surgeon will likely prescribe a physical therapy program to help you regain strength, flexibility, and range of motion in your knee. Following the physical therapy program as directed is essential to ensure the best possible outcome.
Dressing Care
Your surgeon will provide instructions for keeping the incision site clean and dry. Follow these instructions carefully to reduce the risk of infection. The dressing is waterproofed, but you should minimise water contact for the first two weeks. If the edges of the dressing are not sealed anymore, you should attend a medical facility for a dressing change by an allied medical nurse, GP or in your surgeon's rooms.
Activity Restrictions
Your surgeon may recommend specific activity restrictions for some time after surgery. These may include avoiding high-impact activities, sports, and other strenuous activities that could stress your knee.
Follow-up Appointments
You must attend follow-up appointments with your surgeon to monitor your progress and ensure your knee is healing correctly.
Follow your surgeon's instructions carefully and contact your surgeon if you experience any new or worsening symptoms, such as severe pain, fever, or signs of infection. Most patients can expect to return to normal activities within several months after patellofemoral stabilisation surgery with proper care and rehabilitation.
Patellofemoral Stabilisation Prognosis
Generally, patellofemoral stabilisation has a high success rate in improving knee stability and function. Patients may need to wear a brace or crutches for a few weeks after surgery. Physical therapy is essential to the recovery process and can take several months.
Patellofemoral Stabilisation Risks
Like any surgical procedure, patellofemoral stabilisation carries some risks, including
- Infection: There is a risk of infection at the incision site, which can be treated with antibiotics.
- Blood clots: Blood clots can form in the veins of the legs, which can be prevented with medication or compression stockings.
- Nerve Damage: The nerves around the knee can be damaged during surgery, leading to numbness or weakness.
- Knee Stiffness: The knee can become stiff after surgery, making moving difficult. Physical therapy can help alleviate this problem.
What if Patellofemoral Stabilisation is Delayed?
If left untreated, patellar instability can lead to long-term issues, such as arthritis, cartilage damage, and chronic pain. Delayed treatment can also increase the risk of complications during surgery. It is crucial to seek medical attention immediately if you experience patellar instability or recurrent dislocations.