Knee Cartilage Repair
What is Knee Cartilage?
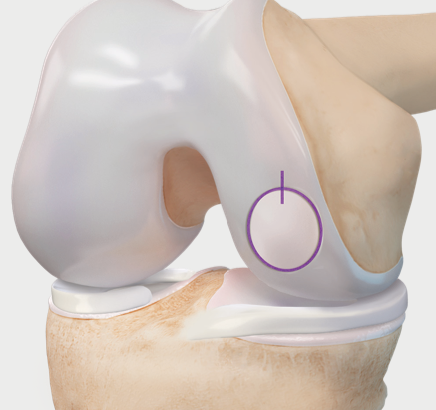
The knee joints are lined by extremely smooth tissue called “articular cartilage.”
The articular cartilage of the knee coats
- the end of the femur (thigh bone),
- the top surface of the tibia (shin bone), and
- the back surface of the patella (kneecap).
It is a protective cushion, allowing smooth, low-friction movement of the joints as one bone end moves on the other. Cartilage tissue covers the adjacent bone surfaces of the knee.
What is Knee Cartilage Repair?
Knee cartilage repair is a surgical procedure that aims to repair or replace damaged cartilage in the knee joint. The procedure involves removing and replacing damaged or diseased tissue with healthy tissue. The procedure seeks to reduce pain, improve joint function, and prevent further damage to the knee joint.
Who is Suitable for Knee Cartilage Surgery?
Most candidates for cartilage repair are young adults with a single injury or lesion. The size and location of the lesion and the status of other knee structures will help determine whether surgery is possible for you.
To improve the chance of success, additional procedures could be recommended. These could include
- Knee Realignment (Osteotomy) and
- Ligament Reconstructions.
Older patients, or those with many lesions in one joint, are less likely to benefit from the surgery, as this process is more representative of osteoarthritis.
Isolated knee cartilage repair may not be suitable for individuals who have:
- Large areas of cartilage damage
- Unstable knee joints
- Poor knee alignment
- Significant arthritis
In these cases, adjuvant procedures might be recommended as well.
What are the Benefits of Knee Cartilage Repair?
The benefits of knee cartilage repair include:
- Reduced pain and swelling
- Improved knee function and mobility
- Prevention of further damage to the knee joint
- Delay or avoidance of knee replacement surgery
Cartilage Repair Procedures
The most common procedures for damaged cartilage are:
- Chondroplasty
- Microfracture
- Autologous Minced Cartilage Implantation
- Matrix-Induced Autologous Chondrocyte Implantation (MACI)
- Osteochondral Autograft/Allograft Transplantation
Chondroplasty
This procedure involves
- Smoothing the roughened areas to create a contained defect
- Removing any loose fragments
Benefits of chondroplasty are that it is not invasive with quick recovery, but it does not stimulate cartilage regeneration. In many cases, patients who have joint injuries, such as meniscal or ligament tears, will also have cartilage damage.
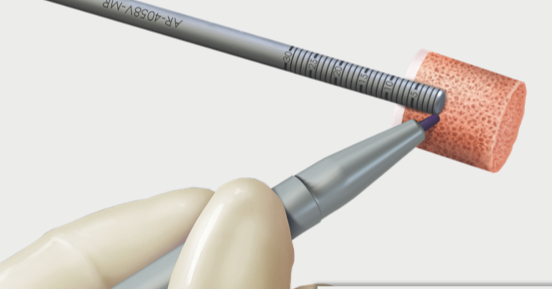
Chondroplasty involves smoothing out any unstable areas of cartilage by using fine mechanical shavers and thermal devices to stabilise loose areas of cartilage.
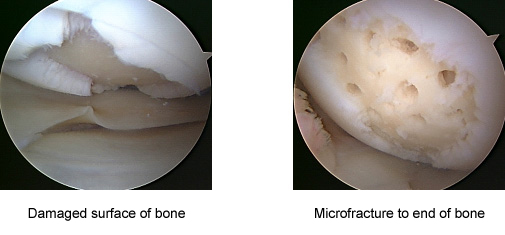
Microfracture
The goal of microfracture is to stimulate subchondral stem cells to create a clot in the defect, which will become fibrocartilage by chondroblast cell differentiation. As with Chondroplasty, this procedure involves
- Smoothing the roughened areas and creating a stable and contained defect,
- Removing any loose fragments, and
- Scraping any exposed bone to stimulate cartilage recovery.
A tool makes multiple holes in the joint surface to promote a healing response. Stem cells from the underlying bone marrow create new fibrocartilage tissue.
This procedure is best for young patients with
- A Single Lesion
- Lesions Under 2cm
- Healthy Subchondral Bone
The recovery is usually slower than a chondroplasty as specific rehabilitation protocols are required to allow the new fibrocartilage to regenerate, such as partial/touch weight bearing for six weeks. Sometimes the procedure can be augmented with fibrin glue to increase the chance of success potentially.
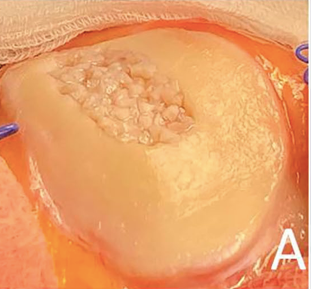
Minced Autologous Cartilage Implantation
It consists of a more modern procedure where the surgeon removes some fragments of cartilage from a non-important zone of the knee, and these particles are implanted in the chondral defect. Microfractures are performed of the same type.
The theory is that this procedure can facilitate the formation of better quality cartilage, such as hyaline, rather than fibrocartilage, as it employs patients' chondrocytes. This would increase the survivorship of the repair and potentially knee function for longer. The procedure is usually augmented with fibrin glue or collagen membrane sutures to maintain the repair in place.
Matrix-Induced Autologous Chondrocyte Implantation (MACI)
MACI is a Two-step procedure.
- healthy cartilage tissue (chondrocytes) is removed arthroscopically
- cartilage cells are sent to the laboratory and grown in vitro
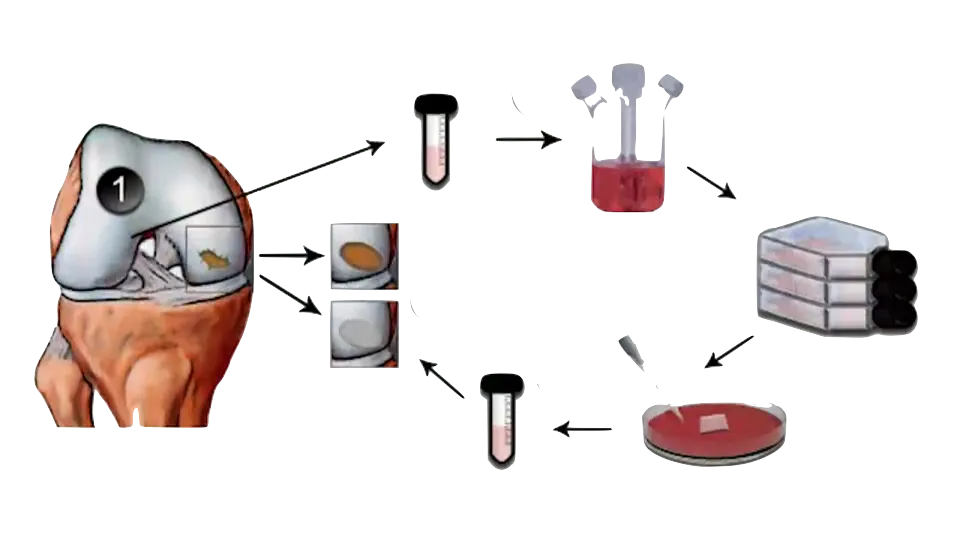
3. The new cells are then implanted back into the patient’s knee. A Collage membrane rich in cultured chondrocytes is implanted into the defect and sutured with absorbable sutures.

The culturing process takes six weeks.
Over time the benefits of this approach are
- no danger of tissue rejection
- theoretically, the implanted material will regenerate hyaline cartilage
This procedure is best for young patients with
- a single lesion
- lesions under 4cm
- healthy subchondral bone
- Normal lower limb alignment
Treatment for an MACI procedure can be costly, and the culturing is not covered by private health insurance. However, it has long-term follow studies proving its good outcomes and still the gold standard of treatment of larger injuries in high-level/ competitive athletes
Osteochondral Autograft/Allograft Transplantation
Autologous/Allograft Osteochondral Transplant is usually recommended when a large defect of bone and cartilage has occurred.
In small Lesions, the donor site can be non-weight-bearing regions of the patient's knee. A single or several small osteochondral plugs are removed from one region (usually edges of the trochlear region) and implanted where the bone and cartilage defect is located. This can also be called Mosaicplasty procedures
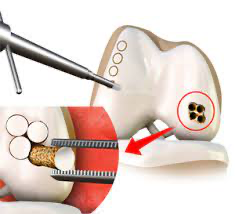
Patients with any plane malalignment as well as those with chronic anterior knee pain or patellofemoral abnormality, might not be ideal candidates
When large osteochondral defects are present (> 4cm), the graft needs to come from a donor, usually from retrieval, and the graft is maintained in sterile solution under -4 degrees celsius for a short period until it is used. This procedure involves a donor and patient anatomy match, and it can take a few weeks/months until the ideal graft dimension is found.
Cartilage Damage Prevention
The best way to keep your knee joint healthy is to
- keep a low body weight
- perform regular low-impact exercises (bike riding, swimming, gym exercises)
- build core muscles by exercise or pilates, especially around your quadriceps and hamstring muscles
Preparing for Knee Cartilage Surgery
Once your doctor decides that surgery is required, preparation is necessary to achieve the best results and a quick problem free recovery.
Preparing mentally and physically for surgery is essential for a successful result.
- Your surgeon will provide you with detailed instructions about how to prepare for the surgery. Be sure to ask questions about the procedure and follow their instructions carefully.
- The better your physical condition, the quicker you recover from surgery. Try to get in shape by exercising regularly and eating a healthy diet.
- Weight loss is always encouraged and recommended before osteochondral procedures, especially when BMI is over 30. Talk to your GP or dietician about getting your weight down before surgery.
- Smoking can hinder the healing process and increase the risk of complications. Quitting smoking at least six weeks before surgery will reduce these risks.
- Before the surgery, your doctor may require a physical exam to ensure you are healthy enough for surgery. They may also order blood or other diagnostic tests to check your health.
- You will need someone to drive you home after surgery and help you with daily activities for the first few days. Make sure you have someone who can assist you.
- Make sure your home is clean and tidy before surgery. You may need to move furniture or install handrails to make it easier to move around.
- You must take time off work to recover from knee cartilage surgery. Talk to your employer and ensure you have enough time off to recover fully.
Report any infections to your doctor before surgery, as the procedure cannot be performed until all infections have cleared up.
After Knee Cartilage Surgery
Some patients need one night in the hospital, although it is possible to leave the hospital on the day of surgery.
After your operation, you will have pain medication and antibiotics.
The wounds take 7-10 days to heal. Most patients improve dramatically in the first two weeks.
If any postoperative problems arise with your knee, such as redness, increasing pain or fevers, do not hesitate to contact your doctor.
When Can I Drive After Cartilage Surgery?
Driving a car is discouraged for 48 hours after anaesthetic. After 48 hours, your ability to drive will depend on the side you had your operation, left or right, the vehicle you drive, manual or automatic, and the type of procedure you will receive. Speak to your surgeon prior, and he will discuss it in detail.
Return to Work After Cartilage Surgery
Return to work varies depending on the procedure performed and the type of work you do. Most patients can return to office work within one week. Labour-intensive work, however, may require up to 6 weeks before returning to complete duties.
During this period, patients are not fit to perform work duties that involve:
- Prolonged Standing,
- Heavy Lifting,
- Bending, or
- Excessive Stair Climbing
Return to Sport After Cartilage Surgery
As the knee joint cartilage has been damaged, activities such as long-distance running are not recommended as this can result in rapid deterioration of the knee joint cartilage.
It is best to delay leisure activities or sports for six weeks to allow the cartilage to heal and repair. However, depending on what type of procedure is needed, more or less time off sports will be required. Your surgeon can provide more detail.
Pain Management
Often, there is little pain they have after surgery. This is because a local anaesthetic is injected around the wound during the procedure and performed arthroscopically (i.e. minimally invasive keyhole surgery).
Outcomes of Knee Cartilage Repair
Knee cartilage repair has a high success rate in reducing pain and improving knee function and mobility. However, it may take several months to a year for the full benefits of the procedure to be realised. Some patients may need additional surgeries or treatments to manage symptoms in more complex cases.
Knee Cartilage Repair Risks
Like any surgical procedure, knee cartilage repair carries some risks and potential complications, such as
- Infection,
- Bleeding,
- Blood clots,
- Nerve damage,
- Chronic pain
- Stiffness or limited mobility,
- Graft failure or rejection
- Osteoarthritis
The risk of complications can be minimised by following the surgeon's instructions before and after the procedure, reporting any unusual symptoms or side effects promptly, and attending follow-up appointments.
What if Knee Cartilage Repair is Delayed?
If knee cartilage repair is delayed, the damage may worsen, leading to more severe symptoms, such as chronic pain, stiffness, and reduced mobility. Delaying the procedure may also increase the risk of complications and the need for more invasive surgeries or treatments in the future.
Therefore, it is essential to consult with an orthopaedic surgeon as soon as possible if you experience knee pain or other symptoms that may indicate cartilage damage. Early diagnosis and treatment can improve the chances of successful knee cartilage repair and minimise the risk of complications and long-term disability.